A.WHAT MATTERS
IN THE SURGICAL ONCOLOGY
General Background
B. UPPER LESION
Surgical Oncology of the Early Bronchial Lesion. The Contribution of
CBC
C. LOWER LESION
Surgical Oncology of the Early Lesion of the Pulmonary Tissue. The
Contribution of CBC
D. THESIS
Concept B CZ
E.
ACHIEVING OPTIMAL RESULTS THROUGH EARLY MULTIDISCIPLINARY CARE IN
PULMONARY ONCOLOGY
A.
WHAT MATTERS
IN THE SURGICAL ONCOLOGY
T. Horvath
Introduction
Surgical oncologist is a peculiar element of the varied community of
the vigorously engaging specialists in the struggle with the lethal
disease. As the surgery is a teamwork par excellence, he knows, that
a chain is as strong as its weakest link: in the spheres in which a
pessimist is crying, which is a situation than I am willing not to
take into account; where an optimist ingenuously bumps against a new
challenge of disease, he ought as a realist to recall the success in
a way “one for all and all for one” arranging matters in compliance
with that and the chain becomes suddenly not to be broken.
Particular components of surgical oncology exist themselves alone –
simultaneously, independently, with the same level of significance –
without superiority or inferiority without merging or separating –
creating a sole integral entirety characterized with a high
difference and a profound equality of their parts. Although each of
them represents specific issue, all of them belong to the specialty.
Surgical oncology would be ranked among the most comprehensive
proficiencies supporting a view of legitimacy of the knowledge unity
concept. That is not a case of golden hands. It is much more
attractive. It includes the delicate handling with tissue and organs
as well the whole patient’s human being. They are harmonized there
the information of multilayered variety of oncogenous processes
categorized by medical and other sciences, natural as well as human,
with an important participation of technologies, with non-negligible
roles of intuition and empiricism – including manual labour. It is
influenced by feedbacks proper to surgery and medicine, in the
widest sense of the words, by statistics, economics, psychology,
sociology and obviously also by politics. Surgical oncology is
created by four parts.
Let’s define the chapters in singles :
I. Surgery of premalignancy
II. Treatment of “surgical stage” of oncological disease
III. Surgery of locally advanced disease:
Palliation, sanitation, devitalization, metaintervention
IV. Surgical treatment of metastatic disease:
IV. a – surgery of solitary metastasis by means of the strategy
identical with the second chapter.
IV. b – surgery of general spreading of the disease, solving a local
problem of the general extent by means of strategy similar to the
saving treatments of the third chapter.
I. Surgery of premalignancy
a) The advanced premalignant changes are signalling a risk of cancer
development in the tissue. Biopsy proof of the severe dysplasia
leads to think about the presence of malignancy in the concerned
focus with the whole appropriate surgical routine of work. b)
Another scenario is represented by mild or moderate dysplasia, at a
given moment clinically insignificant. Their biological development
in the subsequent phase is used to be difficult to guess, especially
at the earlier detections. The context faced dilemma of
overdiagnosis /overtreatment versus underdiagnosis/undertreatment:
- the overdiagnosis represents clinically an irrelevant/insignificant
diagnosis, not requiring any treatment, because it would be
superfluous – overtreatment, as express commonly used terms.
- the underdiagnosis includes all varieties of diagnosis
underestimation, usually in connection with an insufficient
treatment – undertreatment with all consequences. Decision making is
not easy but the surgical empiricism knows a rule of thumb: it is
better to perform surgery unnecessarily than late. An example might
be a diagnosis so “simple” as appendicitis; and a special example
then a pulmonary coin lesion.
II. Treatment of “surgical stage” of
oncological disease
Preoperative counselling in the widest sense signifies offering and
getting of all appropriate information, before an informed consent
of the patient: a) to communicate with the patient, having respect
for all her/his personal (physical, psychical and spiritual),
familiar, professional and social peculiarities. b) to cultivate
permanent relationships with specialists of imaging, medical and
radiation oncology, cytology and histopathology, medicine, clinical
psychology etc., to find an optimal, generally valid and acceptable
solution. That should precede the following steps: c) determination
of one’s own chirurgical strategy d) explanation of general
organisation of the surgical concept and special details referring
to the particular patient e) all of that in accordance with up-to-date
progress in the field of knowledge.
It doesn’t remain as to say, that the strategy of the contemporary
surgical oncology usually recommend to consider radical surgery with
sufficient safety border of healthy tissue by the smallest
biologically acceptable anatomical resection in connection with
regional lymphadenectomy en block – expressed by the term curative
resection.
III. Surgery of locally advanced disease:
Palliation, sanitation, devitalization, metaintervention
Heterogenous surgical interventions there are involved in the third
chapter, all with a common denominator: locally considerably
advanced, radically predominantly insoluble disease. Procedures used
in this category represent prospect for survival of incurable
patient with amelioration of the quality of life. Exceptionally,
they can become to a qualified effort for its radical solution, even
if close to the extreme.
They are represented mainly by non-radical procedures:
1) Palliation – classical examples: the avoidance of inoperable
obstacle of GIT passage by entero-enteroanastomosis, laser
recanalisation of bronchus obstructed with tumour mass, or
artificial reinforcement by stenting of ureter compressed by tumour.
2) Sanitation – the ablation of necrotic tumour mass even in spite
of general spreading of disease, on account of massive secretion, of
pungent odour, threatening to bleed to death
3) Devitalization – trying to dissolve the extensive inoperable
tumours by interruption
of their vascular supply. Even if the argumentation of
devitalization followers is from the point of view of general
oncology in some respects incomplete, its supremely surgical ethos
can’t be neglected. As there is also the case of metaintervention,
below mentioned. Surely under condition of nil nocere. While the
indications of palliation and sanitation are more or less obvious,
devitalization can be always considered an enfant terrible.
4) Radical intervention in the chosen cases of locally extremely
advanced disease with excluded distant metastases represents a
relative novelty. It requires transanatomical access often with
utilization of (auto)transplantation and of artificial materials for
replacement of infiltrated vascular structures. These procedures are
issued from seasoned surgeons in well coordinated teams of top
centres. They have their proponents and also opponents. The
indications are individual. In the essential argumentation compete
technical realizability with biological authority. The internal
strain of this type of conduct, could be perhaps expressed by the
term metaintervention. The fundamental and global motive of this
chapter too, is the life prolongation and improvement of its quality
with an attitude, not at all just formal (!), and of great
importance at any stage of disease: the help is possible. The most
tragic expression of misunderstanding our profession, and under no
circumstances unflagging work at full stretch of the surgical
oncology, is as follows: The surgeon did not know what to do.
IV. Surgical treatment of metastatic disease
Surgery of the metastatic disease is very specific branch of
oncology:
1) More than at the synchronous metastases the treatment of distant
solitary metachronous metastases evokes the access of the second
chapter of surgical oncology. It should represent a complete
resection with a curative intent. The others conclude about
suitability of a simple excision of the lesion in the case of
metachronous lesion, too. Valid data are lacking. A way downwards
cannot be excused automatically. Each case has to be judged
individually in all given correlations.
2) Surgery of general spreading disease, e.g. a wedge excision of
ten metastases of sarcoma to the lung, or the radiofrequency
ablation of five metastatic focuses in the liver in terms of tumour
mass reduction, for instance before perfusion chemotherapy, remains
open. There are both their advocates and opponents.
3) Another category of the management of distant metastatic disease
includes also palliative abdominocentesis for a tumour ascites, or
talc poudrage of the interpleural space for a metastatic pleural
effusion. The same procedures would be used in the part a/ of the
previous third chapter within the bounds of surgical palliation of
the manifestation of locally advanced cancer of relevant organs.
Conclusion
No collective authority of a specialized indicating commission can
remove from any individual surgeon the personal responsibility for
the actual treatment sewed to the patient to measure – it is said
today personalized. Definitive decision is sometimes done at the
most dramatic moment of the surgical procedure. In that sense and in
accordance with the above mentioned, a surgeon is not only a meek
part of a deciding chain, but as an executive agent, he is
autonomous. That does not weaken him; it strengthens him. The more
he is well-educated and skilled, the more he is independent and free
to make correct decisions. Surgery never means a defensive. The
surgery, cheir ergein , means, apart from other things, the well
informed, consequently reserved, nevertheless a strong fortitude to
act.
©C11_DUSOth
B.
SURGICAL ONCOLOGY OF THE EARLY PULMONARY LESION
UPPER LESION The contribution of CBC to the issue
Summary
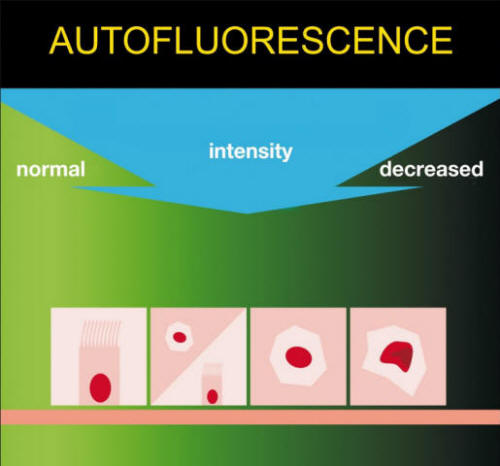
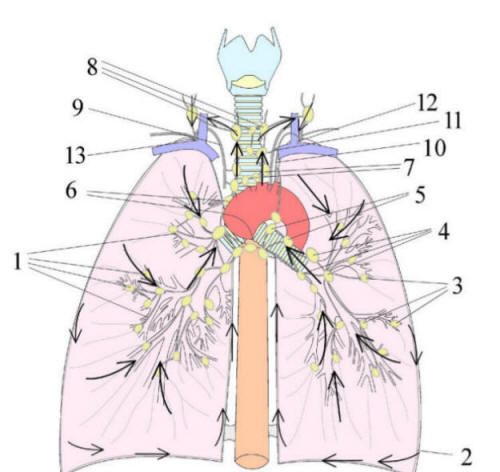
Background: Description of the morphological features of bronchial
carcinogenesis (Scheme 1)
in vivo by use of autofluorescence bronchoscopy.
Patients and methods:
Yearly repeated bronchoscopy in persons (n=361) with high risk of
lung cancer by Autofluorescence endoscopy SAFE-1000 Pentax during
dozen years (1999-2010). Both white light bronchoscopy (WLB) and
autofluorescence (AFB) mode are feasible at the same investigation.
Hematoxylin-and-eosin histopathology and immunohistochemistry p21
and ki67 were used.
Results:
Eleven morphological units of bronchial premalignancy are defined.
They are divided into two classes: Superficial Spreading Lesion – 1/
invisible islet and 2/ spot, 3/ redness islet and 4/ spot, 5/ spider,
6/ swollen and thickened mucosal fold, 7/ granular, 8/ mixed lesion;
and Protruding Lesion – 9/ nodular, 10/ wart-like 11/ polypoid.
Superficial spreading lesions are of high variability. Roughening in
WLB and arenaceous depiction at AFB mode of the surface of the
lesion represent evolving risk of malignant transformation.
Irregular margin of the lesion (star shaped; spider) is important
sign of advanced lesion. Superficial spreading lesions with distinct
limitation (border) represent by histopathology early premalignant
processes. Protruding lesion with smooth surface in WLB and low
decreased autofluorescence signal output is not risky; Protruding
lesion with smooth surface and deep decreased autofluorescence
characteristic is at risk of malignant development or it is
malignant. Wart-like surface of the protruding lesion represents
advanced lesion at risk.
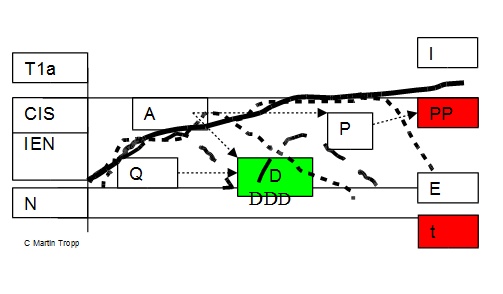
The cogency of overdiagnosis and underdiagnosis issue of every
particular lesion in the course of time were studied (Scheme 2).
There are defined three classes of the lesions regardless of their
superficial spreading or protruding nature in general: 1/ Quiet –
oncologically unimportant, in the course of time disappearing lesion
2/ Ambiguous – representing biologically uncertain unit inviting
follow-up endeavour, and 3/ Persistent – proliferative lesion at
risk needed particular attention from the clinical point of view.
Conclusion:
To detect early bronchial premalignancy low output ilumination
intensity and mild autofluorescence signal amplification are needed.
A part of advanced premalignant bronchial lesions at risk is
recognizable by naked eye.
KEY WORDS:
Autofluorescence; Bronchoscopy; Carcinogenesis; Morphology.
Scheme 1. Principle of Bronchial Dysplasia Detection
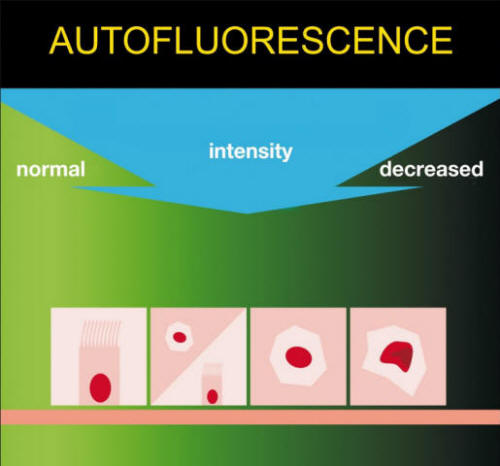
© Ján Otradovec
Scheme 2 Overdiagnosis and
Underdiagnosis
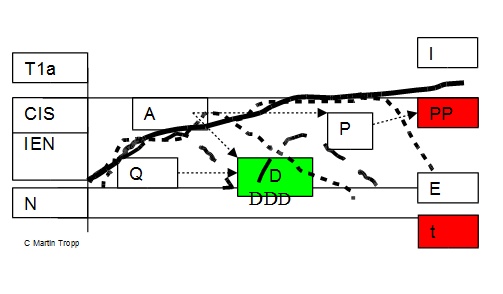
N – normal
epithelium IEN – dysplasia CIS – carcinoma in situ
T1a – superficial
cancer t – time E – epithelial stage of the disease
I – intersticial
spreading of the disease
Lesion:
P – proliferative

A – ambiguous

Q – quiescent

PP
– persistent proliferative lesion at risk
D – disappearing lesion
C.
SURGICAL ONCOLOGY OF THE EARLY PULMONARY LESION
LOWER LESION The contribution of CBC to the issue
Summary
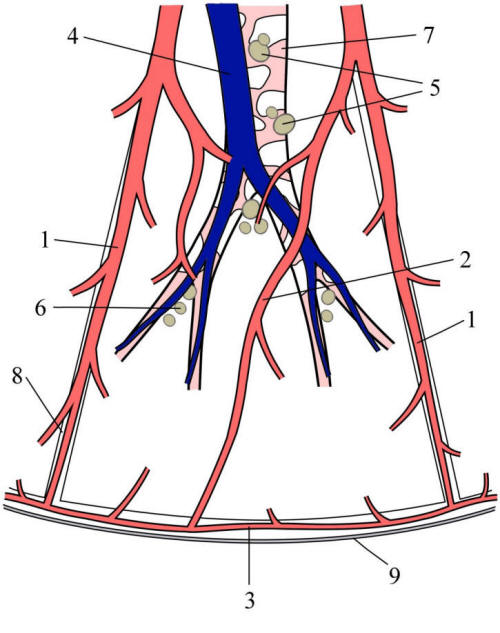
Background: Czech pioneering of pulmonary segmentectomy for cancer.
Patients and methods: Pulmonary opacity suspect of lung cancer
without enlargement of lymphnodes on CT imaging was detected in
twenty persons from high risk group (n=305) by follow up through
5127 examinations during the period of 1999-2008 yrs. Proven non
small cell lung cancer and tumours of uncertain histopathology with
diameter up to 20mm were indicated to segmentectomy (Figure 1).
Borderline diameter for segmentectomy of a metastatis was 30 mm.
They were implemented twenty one Overholts procedures. The
histopathology was stated under hematoxylin-and-eosin staining and
immunohistochemistry examination.
Results: Nine non - small cell lung cancers, six metastases, and six
benign lesions were found histopathologically. No local recurrence
and no involvement of regional lymphnodes were recorded
postoperatively in both cancer series with median age of 63 yrs (range
45-79) and median duration of follow up 35 months. No perioperative
30-days mortality was registered. Six distant recurrences appeared,
3 in NSCLC and 3 in extrapulmonary cancer patients. Five cancer-patients
died, three of them through the general progression of the disease,
two deaths were non-cancer related. Patients with NSCLC represent 1‰
among all operated Czech pacients with lung cancer of the period.
Conclusion: Lung segmentectomy seems to accomplish local control of
early stage NSCLC and pulmonary metastasis of extrapulmonary cancer.
Broad multidisciplinary collaboration focused on early stage disease
is needed.
KEYWORDS: Early Lung Cancer; Segmentectomy; Lymphadenectomy.
Figure 1 Scheme of the Surgical Lung Segment
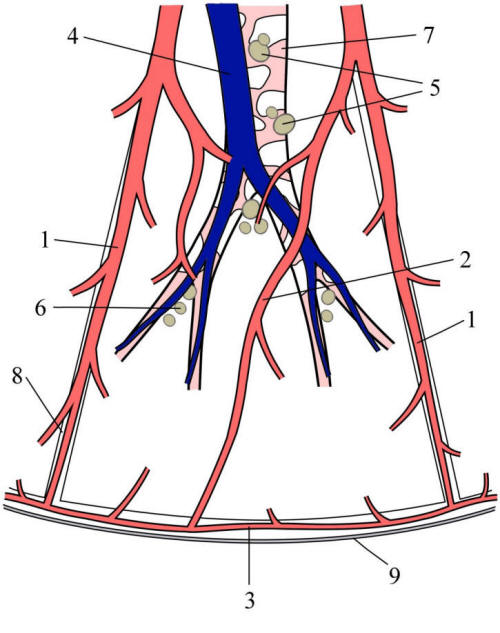
©
Marek Malik
Legend:
1
intersegmental pulmonary vein
2
intrasegmental pulmonary vein
3
subpleural pulmonary vein
4
pulmonary artery segmental branch
5
segmental lymphnodes
6
subsegmental lymphatics
7
segmental bronchus
8
intersegmental space
9
visceral pleura
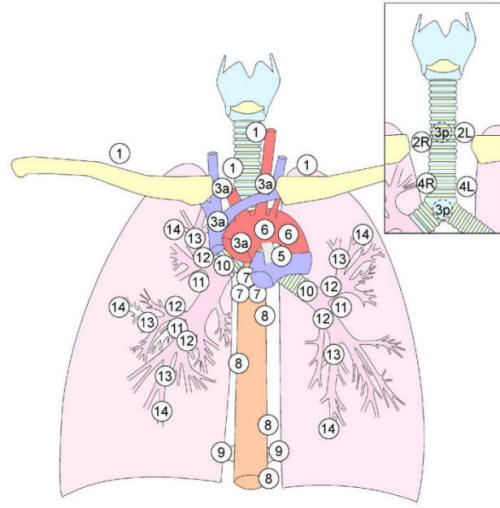
Figure 2 IASLC Scheme of Thoracic Lymphatics
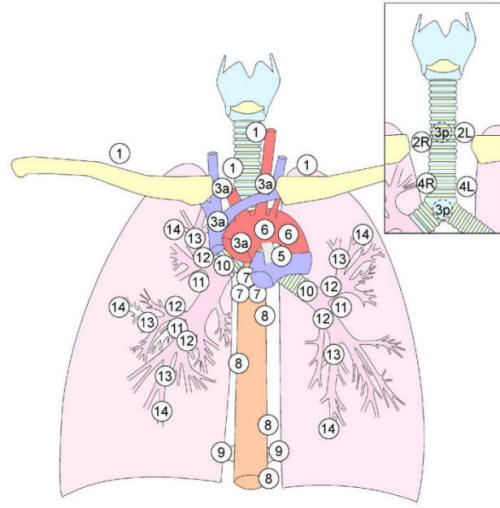
©
Marek Malik
Legend:
1 Lower
Cervical, Supraclavicular and Jugular
2 2L
Upper Paratracheal Left 2R Upper Paratracheal Right
3 3a
Prevascular 3p Retrotracheal
4 4R
Lower Paratracheal Right 4L Lower Paratracheal Left
5
Subaortal (Aortopulmonal Window)
6
Paraaortal (Ascending Aorta, or Phrenic )
7
Subcarinal
8
Paraesofageal
9
Pulmonary Ligament
10
Hilar
11
Interlobar
12
Lobar
13
Segmental
14
Subsegmental
Figure 3 Anatomical Scheme of the Lung and Mediastinal Lymphatics
Lymphatic Stream
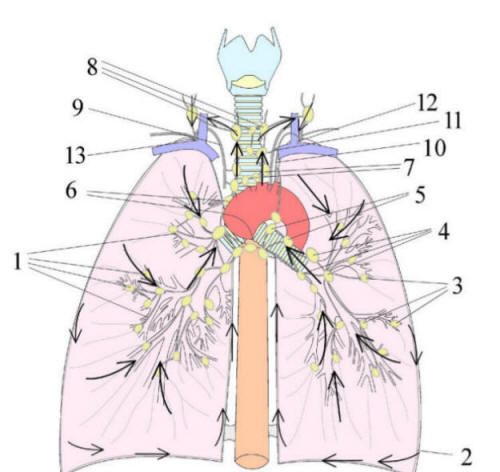
© Marek Malik
Legend:
1 deep lymphytics
2 ubpleural lymphatics
3 pulmonary lymphatic nodes
4 bronchopulmonary lymphatic nodes
5 hilar lymphytic nodes
6 tracheobronchial lymphatic nodes
7 lower paratracheal lymphytic nodes
8 upper paratracheal lymphytic nodes
9 right bronchomediastinal lymphatic trunk
10 left bronchomediastinal lymphytic trunk
11 thoracic duct
12 left venous angle
13 right venous angle
D.
THESIS
Lung cancer – preventable disease. A surgical view.
Concept B CZ Horvath T. & Horvathova M.
I. Introduction
Lung tumours are located in two anatomically distinct regions – in
the central airways (upper lesion) and in the pulmonary parenchyma (lower
lesion). They demand different diagnostic and therapeutic tools.
Diagnostic modality of upper lesion is bronchoscopy. Lower lesion is
detected by imaging, especially computer tomography (CT). Key note
of the prevention and early diagnosis fall within of authority of
epidemiology and public medicine. The most efficient method of the
treatment is surgery. Treatment methodology of proximal lesion is
partly represented by therapeutic bronchoscopy, greater part of it
is dominating by surgery. The treatment of distal lesion is surgical.
Being efficient surgery needs effective diagnostics by imaging,
endoscopy, and histopathology. The more are they integrated into
surgical oncology (it goes without saying the more is a surgical
oncologist involved into the professions most close to her/his
profession) the closer to the entirety of goal seeking. Respect to
the category of the lesion is neded to reach a solution adequacy in:
A. premalignant B. primary pulmonary malignancy C. pulmonary
metastasis.
A.
Endoscopically detectable premalignancy has a suite of morphological
features, but three biological variantions only: 1/ persistent
proliferative lesion at risk 2/ ambiguous intraepithelial lesion in
a part progressing in the course of time to the risky dysplasia or
regressing back to normal mucosa 3/ transient quiet lesion,
disappearing in the course of time. Long term monitoring of the
finding discloses the biological character of the tissue
differentiating clinically important and unimportant lesion (over/under-diagnosis
issue). To diversify clinically important and inconsequential
finding is assisted by accumulation of certain measure of experience.
That precedes an undervaluation of the manifested initial
asymptomatic weighty development – underdiagnosis – or its
overestimation i.e. overdiagnosis. They might lead at the same time
to the undertreatment – meaning insufficient therapy; or to the
overtreatment – i.e. superfluous therapy.
Endoscopically detected malignancy is treated mainly surgically.
B.
Technically and biologically operable primary pulmonary tumours
detected by imaging and endoscopy represent the field for radical
surgery of the lung (classic, videoassisted, robotic) in the
“surgical“ stage of the disease: i.e. anatomical resection,
sufficient margin of healthy tissue, adequate lymphadenectomy.
Sooner the better, but extreme cases tackle a question of
overdiagnosis and led-time bias.
Surgery of the peripheral nodules argues with relevance or
irrelevance of the diagnosis (under/overdiagnosis) lead time bias
including, and with the justification of surgical intervention.
These are discussed with the context of less agressive properties of
a part of detected peripheral pulmonary lesions and with the role of
the lymphatics in the spreading of more agressive tumours.
C.
Solitary metastatic pulmonary tumour is an object for radical
resection with identical technical premises mentioned above (being
aware of permanent dilemma of overtreatment enthroned).
Radical anatomical procedure with regional lymphadenectomy
alternating wedge resection without lymphadenectomy are used. There
are no EBM arguments to the recommendation of regional
lymphadenectomy in the case of metastasis. Some background warn
against its overall refusal .
Lobe specific lymphadenectomy is according contemporary ESTS
guideline and IASLC recommendation inseparable part of the curative
pulmonary resection of NSCLC. The premise of the united proceeding
is represented by the IASLC map of pulmonary and mediastinal
lymphatics.
II. Upper Lesion
Individuals from a mixed cohort of persons with high risk of lung
cancer were more years investigated periodically. In vivo
manifestation of varied optical and morphological features of
bronchial intraepithelial neoplasia (dysplasia) using System
Autofluorescence Endoscopy SAFE-1000 Pentax was studied.
They are descibed twelve morphological units classified into six
groups. They represent three manner of biological behaviour
mentioned above. As a result of the endeavour was found a
surprisingly simple fact that persistent lesion shows the signs of
proliferation by ki67 and p21 immunohistochemical investigation. It
is at risk. Because it is relevant and necessary take it out.
III. Lower Lesion
Starting to cultivate Czech clinical culture of pulmonary
segmentectomy for tumour up to 20 millimeters in diameter in
junction with regional lymphadenectomy since its scientific
confirmation years ago we are advocating it to date still as unique
subject in the state. That accounts for the part of 1 per mille of
the lung cancer surgical procedures in the Czech Republic in the
monitored ten years time period 1999-2008.
Facultative indication of pulmonary segmentectomy for primary non-small
cell lung cancer represent small peripheral tumour up 2 cm in the
diameter with a margin of healthy tissue wider than 1 cm providing
normal preoperative finding
on the thorax CT scan on the pulmonary and mediastinal lymphatics
and negative histopathology of the lymphatic nodes. We are detected
the tumours in the risk group by ourselves. There are not registered
local recurrence with folloow-up median of 35 months.The metastatic
tumours are indicated up to 30mm in the diameter for resection.
Pulmonary and mediastinal lymphatics were classified by Naruke. It
is used IASLC lymphatic map a common scheme of general acceptance
recently. There are in the IASLC scheme described 14 stations of
thoracic lymphatics divided into 5 categories and 7 zones:
Supraclaviclar zone # 1 SUPRACLAVICULAR NODES; Upper zone # 2,3,4;
SUPERIOR MEDIASTINAL NODES AP zone AORTIC NODES # 5,6; INFERIOR
MEDIASTINAL NODES Subcarinal zone # 7; Lower zone # 8,9; N1 NODES
Hilar / Interlobar zone # 10,11; Peripheral zone 12,13,14;
IV. Thesis Resource
The optimal access to lung cancer is represented by primary,
secondary and tertiary prevention focused onto risk groups. It is
connected with early diagnosis and treatment, the entirety of a
longstanding follow-up including. In a carefull follow-up
examination is founded high potential to the detection of
synchronous or metachronous extrapulmonary tumour duplicities and
lung involvement with metastatic disease too. Disclosing and solving
of non-oncological problems of surgical and medical nature made
easier.
A complicated and very interesting issue is concerned: on the very
horizon of full endeavour emerges a catch of sight of lung cancer
curability paradigm.
V. THESIS
FOCUSING EARLY DETECTION ON ADEQUATE CATEGORIES OF PERSONS AT RISK
OF LUNG CANCER CONNECTED WITH EARLY THERAPY OF THE FINDINGS
FACILIATES PROLONGED SURVIVAL, IMPROVEMENT OF THE QUALITY OF LIFE,
FINANCIAL SAVINGS IN THE SYSTEM OF MEDICAL INSURANCE AND MANY-SIDED
PERSONAL, FAMILIAR, PROFESSIONAL AND SOCIAL ADVANTAGE.
E.
ACHIEVING OPTIMAL RESULTS THROUGH EARLY MULTIDISCIPLINARY CARE IN
PULMONARY ONCOLOGY
Teodor Horvath
BACKGROUND DEFINITION
Early management of lung cancer continues to be one of cardinal
questions of pulmonary oncology. Scientific knowledge of relatively
self-contained space of early diagnosis and therapy are searched,
checked up and classified in cooperative field of histopathology,
pneumonology, radiology and surgical oncology. Basic information is
acquired by the research in the risk groups. Comparing the results
sourced by different methods and/or with the situation in non-risk
population is defined the difference. Verrified data represent
rational basis to advance suggestion for modification of the
standard algorithms
HISTOPATHOLOGY OF THE PULMONARY ONCOLOGY
Multistep process originating pulmonary adenocarcinoma (ADL) –
adenocarcinogenesis – is illustrated through mapping of allelic
imbalance of 25 selected genes by Masayuki Nogutchi. The progress of
adenocarcinoma in situ (AIS) to early invasive adenocarcinoma (EIA)
is considerably supported by participation of abnormal demethylation
of stratifin (SFN).
Peripheral ADL is on the CT imaging presented by ground glass
opacity (GGO). Cavita Garg analyses the controversies of the
clinical management of GGO by correlating histopathology of ADL with
HRCT imaging of three GGO essentials – pure GGO, GGO with solid
part(s), and solid lesion. They are presented in numerous variable
forms. She emphasizes the need of multidisciplinary teamwork on
their classification with the aim of desirable general guide.
Similar appeals are heard from many sites. They might not be
disregarded as accidental. Further examples referred to necessary
multidisciplinary cooperation are strict differentiation of the
biological behaviour of particular forms of non-small cell lung
cancer (NSCLC) i.e. among squamous cell lung cancer (SQL), ADL, and
their mixed forms, pulmonary carcinoid (CAT) and other kinds of
pulmonary neuroendocrine tumours (PNET), exact definition of less
and high agressive forms of small cell lung cancer (SCLC) and giant
cell PNET, clear correlation of their incidence with smoking and
additional risk factors. That all seen in real efficiency of the
bronchology, radiology, aspiration cytology, small or greater biopsy
samples, and surgery with final diagnosis of the resecate by
immunohistochemistry.
Horizontal integration is not limited on sparse institutions only,
but it represents a general tendency. Despite of the fact that high
level resolution cannot be achieved by those which have other
problems than complicated cases.
Signalized by the finding of severe dysplasia (SD) or carcinoma in
situ (CIS) pertinent SQL should be anticipated anywhere in the lung
location. With a probability of 80% SQL will evolves in the detected
lesion in a time period of 2-3 years. It happens on the basis of
numerous abnormalities counted minimally twenty genetic and
epigenetic alterations of various chronology and kinetics according
conclusions of Sylvie Lantéjoul. The survey continues about the
development of ADL: from preinvasive atypical alveolar hyperplasia (AAH)
in the typical CT appearance as pure GGO with need of follow up only,
up to the adenocarcinoma in situ (AIS) in fact ex-bronchioloalveolar
cancer (BAC) finally up to microinvasive forms of peripheral ADL,
most frequently seen as a non-solid peripheral pulmonary opacity.
Its character is variable. Onto the biological make out of the
lesion take part both West (Keith M. Kerr, Wiliam D. Trawis), and
East (M. Noguchi). Recent information declared that mucinous
adenocancer of the lung is probably separate nosologic unit.
Wide histopathological engangement does not interfere with simple
direction for surgical handling. It is enabled by this, in contrary.
The indication for surgery is in principle represented by any long
lasting GGO with a development to a non-solid appearance.
Diffuse interstitial proliferative neuroendocrine cells hyperplasia
(DIPNECH) is an autonomous chapter of histopathology of the
preinvasive pulmonary lesion, a precursos of carcinoid. Even
experienced histopathologists studying signs of the lesion face
temptation to assume that DIPNECH might be a precursos of SCLC,
perhaps only some its forms. If is it the case of the less of most
agressive form according clinical observation? Nobody knows. The
issue is an item of sharp disputes (regarded desirable) and of deep
study (regarded needful).
BRONCHOLOGY
In the clinical field of early lung cancer is bronchology
represented by autofluorescence bronchoscopy (AFB) . Is it an
important diagnostic tool or not ? Is the clinical benefit of the
method predominated over the time, economic and technic limitations
? No, they are not predominated over. The AFB is a specific tool
established to detailed identification of detected lesion(s), and
areas estimated for minimally invasive therapy, in patients with
lesions multiplicity (synchronous and metachronous) and the follow
up care in the risk group. Is there a need of technical enhancement
? Yes, of course. It undergoes a development similar to any other
method, concludes Eric Edell.
CLINICAL SYNTHESIS THROUGH IMAGING
Notable information based on the recent released results from the
National Lung Screening Trial (NSLC) sponsored by the National
Cancer Institute of the United States is pointed out by John K.
Field: Claudia Henschke with coworkers showed, that lung cancer
deaths was reduced by 20% and all-causes mortality reduced by 7%
when smokers defined as former and current smokers with 30 or
greater pack-years of smoking were screened regularly using low-dose
spiral CT compared with standard X-ray.
The commentary to NLST of Giulia Veronesi “Hypothesis of
overdiagnosis is undermined“ speaks eloquently to the supporter,
irresolute or opponent of the method.
See www.nejm.org/doi/full/10.1056/NEJMoa110283 (1) or http://iaslc.technetrics.com/policies/statement-on-ct-screening
SURGERY
The surgical statement for the management of early lesion is
theoretically and technically clear. Curative surgery is represented
by anatomical resection with regional lymphadenectomy. One can
reflect segmentectomy for small tumours up to 20 mm in diameter onto
the basic practical level. Greater tumours are indicated to
lobectomy. In the surgical pool are offered classical open and
videoassisted procedures. The replenishing of the arsenal is
continual by the development of both its parts. The value belongs to
the lymphadenectomy is accented. The finding should be staged as
accurately as possible. The classical procedures are refilled with
TEMLA ( transcervical mediastinal lymphadenectomy) by Marcin
Zielinski a method prerequisite for cervical pulmonary lobectomy.
Videoassisted mediastinal lymphadenectomy (VAMLA) cultivated by
Martin Hürtgen and coworkers represents good tested stil attractive
novelty of the miniinvasive line.
The surgery is reliable, effective and economical therapeutic
instrument. Its fundamental advantage is represented with radical
solution. The surgeon might lose the way in the abundance of
molecular biological data by forgetting one of the best rules of the
art … to operate rather uncesessarily than late.
There is everytime something for doing better in the organization
chart. The importance of team work demonstrates concrete example
from United Kingdom by Kevin Wing Lan. Surprisingly 58% of British
hospitals performing thoracic surgery deal with only one thoracic
surgeon. No surprise that regions with carefully worked-out level
hierarchy starting basic through extension personal and technical
equipment up to top centres with skilled teams and wide technology
background show better perioperative and long-term results.
The progress move along to robotic pulmonary surgery in the actual
western (Bernard Park, Kemp Kerstine) or eastern (Hyun-Sung Lee)
presentation. One cannot neglect importance of stereotactic body
radiation therapy (SBRT) in the comprehensive declamation of Dirk De
Ruysscher especially in functionally or medically inoperable
patients, despite of an imperfection in the reasoning with sets
without complete histopathology.
EPIDEMIOLOGY
Little data exist regarding causation of lung cancer in non-smokers
(approximately 25% of the incidence). It is caused in contrast to
smokers by other biological mechanisms. Preferred population are
women of younger age. It originates probably endemically too, e.g.
in some areas of China. Lung cancer of non-smokers is conditional on
genetic determinants and enviromental components. There are examined
only partially or non-examined. Beside radon and asbestos figure
among the causes hormones, viruses, coal smoke, and kitchen
exhalation. There is accepted the clonal theory of the origination
from one cell but the non-clonal possibility too. Closer elucidation
of the matter will need further united endeavour with great
application.
(2)
CONCLUSION
Through the standard wrestling of neophilia with neophobia one can
observe in the pulmonary oncology that checking old estimation from
new angle of view benefits the knowledge. The opportunity for
effective solution so far seemingly non-soluble problem finally
emerged. Are we ready?
REFERENCE
1)
Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic
ScreeningThe National Lung Screening Trial Research Team N Engl J
Med 2011; 365:395-409
2)
Supplement to Journal of Thoracic Oncology 2011;6 Book 1,2.
ABBREVIATIONS
AAH atypical alveolar hyperplasia
ADL adenocarcinoma of the lung
AFB autofluorescence bronchoscopy
AIS adenocarcinoma of the lung in situ
BAC bronchioloalveolar carcinoma (=AIS)
CAT carcinoid tumor / typical carcinoid
CIS carcinoma in situ
CT computer tomography
DIPNECH diffuse intersticial proliferative hyperplasia fo
neuroendocrine cells
GGO ground glass opacity
HRCT high resolution computer tomography
EIA early invasive adenocarcinoma of the lung
LDsCT low dose spiral computed tomography
NLST National Lung Screening Trial
NSCLC non small cell lung cancer
PNET pulmonary neuroendocrine tumour
SBRT stereotactic body radiation therapy
SCLC small cell lung cancer
SFN stratifin
SD severe dysplasia
SQL squamous cell lung cancer
TEMLA transcervical mediastinal lymphadenectromy
VAMLA videoassisted mediastinal lymphadenectomy
up
|